The Polish Science Voice: Scrutinizing Pain
Read the interview with Katarzyna Starowicz-Bubak, Ph.D about our Pain project in Lider program. “Interaction between endocannabinoids and endovanilloids as a new therapeutic target in neuropathic pain” project financed by the National Center for Research and Development (NCBiR) under its Lider program, Kasia talks to Karolina Olszewska.
What does the “new therapeutic target” in the name of the project mean?
We aim to show what systems, receptors and molecules can be influenced to heal and relieve pain. As a result of the project no new injection or pill will be developed that would be available in pharmacies after the research is completed. Instead we will identify the molecules that will best confirm our research hypothesis. We will also examine their pharmacological properties. We will chart out a new line of research or way of developing drugs for pharmaceutical companies. This stage of research is not about licenses or patents. Our findings are being financed from public funds and we are sharing them with the international research community through publications.
Let’s explain to readers some of the terms in the name of the project. First of all, what are cannabinoids?
This group of substances includes compounds naturally occurring in hemp seed (Cannabissativa) as well as their manmade equivalents. The human body also produces these compounds, so we call them endogenous cannabinoids, or endocannabinoids. One of these is anandamide, an analog of tetrahydrocannabidiol (THC). These compounds are mainly responsible for the regulation of motor functions and the processes of learning, memory and appetite control. However, their role in the regulation of pain perception is also extremely important.
What is this role specifically? When do we feel less pain or when are we in greater pain?
Endocannabinoids are produced in living organisms, including invertebrates, for example snails. In the human body, they have a big impact on many physiological and psychological processes. Among other functions, they inhibit pain signals received by the body. However, there is a problem. If we administer them to the body, they will activate cannabinoid receptors wherever they reach. And that’s not good because there are such tissues and organs where it would be better if these receptors were not activated. For example, these include areas of the brain associated with memory and cognitive abilities. They may produce adverse effects there, such as drowsiness, addiction or psychotic symptoms. A pain impulse travels from where the tissue was damaged (for example, in an arm or a leg) through nerve fibers and the spinal cord all the way to the brain.
Our work focuses on maintaining the analgesic [pain-killing] properties of compounds while avoiding the undesirable consequences associated with a narcotic effect. We want to stimulate cannabinoid receptors only where there is pain—in specific locations. This is one of the strategies for countering pain with the use of compounds produced by the body.
Isn’t this a ready-made recipe for a painkiller?
Unfortunately not. This is due to the specific way in which the human body functions. Endocannabinoids appear in the body on demand, which means when a given cell or tissue needs them. Beside signaling molecules, this system also consists of enzymes. They influence the emergence of the compounds in question and subsequently their distribution. Cannabinoid molecules, for example anandamide, which is at the center of our research, disappear from the environment as soon as they do their job, because they are broken down by the body. And it is their short life span that is the biggest problem in using endocannabinoids as painkillers. Researchers in many laboratories around the world are looking for ways to inhibit their breakdown. If this succeeds, we will achieve a higher concentration of the desired substance in the area where pain is felt—and thus the desired analgesic effect.
So no one has ever managed to develop such a drug?
A promising substance has been developed that is at the stage of tests on patients. The drug increases the level of anandamide and relieves various types of pain affecting peripheral organs. It does not produce psychoactive effects. Unfortunately, studies conducted on patients with rheumatoid arthritis show that this compound does not work for them. It seems that thanks to research conducted under the Lider program we have pinpointed the culprit for this state of affairs. Our research shows that if we block off one path through which this compound breaks down, other degradation pathways become activated. In its complexity, the human body responds quickly and tries to replace the excluded system with something else. To make matters worse, the launch of alternative breakdown mechanisms leads to the emergence of a compound with the opposite effect to what we want. And that means that compounds are produced that enhance the feeling of pain by affecting vanilloid receptors. And this is where we come to the next scientific term included in the title of the project.
Does this mean that the vanilloid system gets in the way of achieving an analgesic effect?
Yes. And that’s why it’s necessary to prevent it from becoming activated. In an article we published in 2013 in the Plos One journal, we have shown why such a magic pill targeted at one particular receptor is not the best option. It is better to have compounds affecting several systems. The results of our observations were confirmed by research conducted by a group led by Prof. Vincenzo Di Marzo from Italy.
How do you study pain?
We are working with both acute and chronic pain models. The pain itself when it appears is a good phenomenon. It warns us that there’s something wrong with us, so we should go to the doctor. After the tissue heals and there is no longer the cause and effect of the damage, acute pain should stop. Sometimes, however, there is excessive damage to nerve fibers, and the brain is still getting pain signals. If this lasts more than three months, that’s chronic pain. One of its forms is neuropathic pain. It poses a challenge for both pharmacologists and physicians. It has a complex and not fully understood mechanism and many components involved in the formation and transmission of the pain response. Complex treatment is needed and the pain is sometimes resistant to the analgesics administered. It is on this model of chronic pain that we are testing a compound that has a two-pronged effect: it increases the level of anandamide in the body (because it inhibits its breakdown), while blocking the vanilloid receptor which exacerbates pain. We are conducting this part of the research on rats. We are assessing pain using behavioral tests, for example responses to tactile stimuli. We are using threshold pain stimuli in the research—or only tactile stimuli, which in some pathological conditions induce an avoidance response. In addition, we are conducting research with a view to getting an insight into molecular mechanisms associated with the development of this pathology.
When can patients with permanent pain expect to be provided with an effective drug?
The research is nearing completion. We are close to demonstrating that a multi-track approach—polypharmacology—is a good strategy for pharmaceutical companies. This is the way to design research and look for effective drugs. Drugs should have an effect on several systems instead of just one specific system. Meanwhile, transforming a molecule into a drug by confirming its clinical properties and safe use for specific conditions, ailments or indications—that’s the job of pharmaceutical companies.
How much has your research cost?
The National Center for Research and Development (NCBiR) has allocated zl.989,000 for our work. Almost half of this amount has been spent on setting up the research team and on salaries. Our work has resulted in a number of publications and conference reports.
Source: http://www.warsawvoice.pl/WVpage/pages/articlePrint.php/27604/article
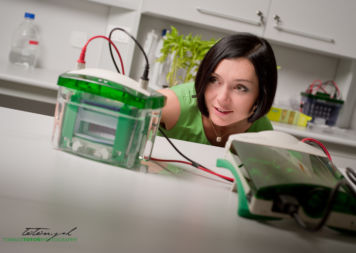
Photos: Tomasz Totoń